One of the most striking features of this utterly brilliant Commonwealth Games has been the dominance of Welsh competitors. Very occasionally this has shown itself through the winning of medals but, most often, it has been through that most highly prized of awards – the moral victory. It is only fair to reflect, however, that Wales also provided one of the negative stories of the Games when the hurdler Rhys Williams, 30 year old son of legendary Welsh winger JJ Williams, failed a drug test. It’s fair to say that this shocked me to the core. How I asked myself could JJ, hero of the 1974 Lions, wing partner to the incomparable Gerald Davies, a man whom I vividly remember watching in his spring-heeled pomp, have a 30 year old child? The answer is devastating in its simplicity; the 70s were long ago and I’m getting a bit old.
I’m not alone. The ageing of our population seems sometimes to be talked of in the same tone as peak oil or an ice free arctic, something that should worry us certainly, but also an issue that will affect us sometime in the reassuringly distant future. But for Dumfries and Galloway, such complacency would be utterly misplaced. We are in the front line of the most profound demographic change that western society has ever experienced; it’s happening now, and it’s happening in Dumfries and Galloway more dramatically than in any other region in Scotland.
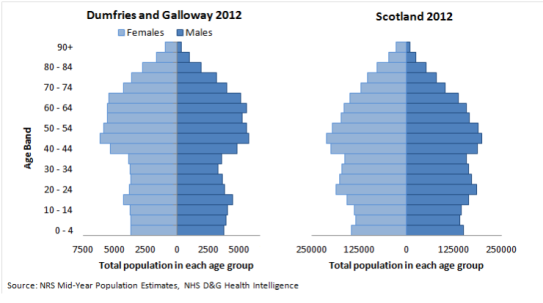
Here’s our population pyramid compared to that of Scotland as a whole.
It’s immediately clear that the term ‘pyramid’ is a misnomer. We have a bulge of population in the older age groups that overshadows the population of children and younger adults. Year by year this bulge is moving up through the age bands, causing a shrinkage of the working age population and an increase of those in the over 65, 75 and 85 age brackets. This is not a far future phenomenon; this is happening to us now and will be the dominant issue in determining the shape of health and social care provision until the population distribution broadly stabilises in the mid 2030s. Ken will do a blog to mark this event (probably beamed straight into your brains by the grandchild of Twitter).
At this point, I was going to start talking about the pressures on health and social care generated by this population shape. I will come to this, but first I think it’s important to say how truly wonderful it is that we’re able to present these figures. What we see here is an absolute triumph of post war healthcare in Britain that’s allowed people to live longer, healthier lives than ever before. We have made enormous progress in reducing mortality from big killers such as stroke, heart disease and cancer and this rate of improvement does not appear to be slowing. A population that’s older than ever before is an achievement to celebrate and something that our clinical and support teams should regard with a sense of pride.
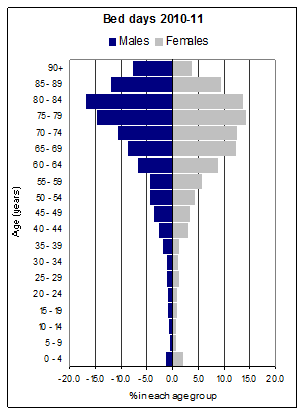
Having said that… Here’s a diagram showing the relationship between age group and the usage of acute beds (expressed as proportion of total ‘bed-days’) at the moment. It’s very evident that age is currently a key driver in hospital occupancy, a fact that becomes somewhat uncomfortable if we think back to that population bulge moving inexorably upwards. And remember that over 80% of health contacts take place outside the acute sector so this profound shift in demand is affecting every aspect of our care.
Essentially, we have a health and social care system that is not designed for the unprecedented demographic change now underway. We will need to change and change both rapidly and radically. On the single issue of acute bed use, for example, we will need broadly to reduce that correlation between age and bed days by around 40% over the next 15 to 20 years. This is a scale of change similar to that undertaken by mental health services over the past decades, but is something never before evidenced in acute care.
There are good reasons to be optimistic about our capacity to deliver this change. One of the most important of these is the forthcoming integration of health and adult social care services. The model, already approved by Council and shortly to be presented to Health Board, will see all of health and adult social care brought under one management structure. This should create far greater flexibility for teams in addressing problems such as delayed discharges. Integration is not a cure-all solution but, if we get it right, it should enable a wider range of solutions to be identified and implemented within localities that will allow our older population to be cared for where safe and appropriate outside of an acute setting.
This is, however, an optimism based on a mechanistic modelling of the future numbers and patient flows. That’s all very well. But, whilst important, it’s not how our service will be assessed or how we should judge ourselves. Our success should instead be measured by the quality of care and support that we deliver to this changing population. I’ve recently completed the Dementia Champions training programme (a superb course which I’d recommend to anyone who has the chance to participate). The programme makes us confront areas where our service does not meet the needs of this vulnerable group or their carers. In one module, for example, we spend a day with current carers of people with dementia discussing their recent experiences and the difficulties they’ve faced in accessing properly coordinated and effectively tailored support. In others, clinical experts present latest thinking on issues such as the quality of pain management or the progress in improvements in end of life care.
There are some great local examples of outstanding person centred care for this patient group. But there is also overwhelming evidence that there is a long way to go to ensure that we reliably provide the level of support to individuals and their carers that maximises potential for independent living and tailor hospital experience to meet individual needs. Some of this we can address relatively easily (give or take £200M); the new acute hospital opening in just 3 years time is being designed using latest thinking on dementia friendly design and will provide a far more appropriate environment for the care of patients with degrees of confusion or dementia. But the much more significant change required is to shape the care provided by health, social care, independent and third sectors in a way that is most effective for that individual, their families and their carers. To do that, we will need to increase the depth of knowledge about our individual patients and their circumstances to a degree that feels daunting in a future of ever shorter hospital stays. It’s a future that will require far better information sharing between agencies and a level of coordination between care providers that is nowhere near reliable at the moment. The integration of health and adult social care gives us a great start on this journey, but there’s an awful lot of redesign still to be delivered.
I think this ambition to transform dementia care is important not only because it’s so plainly the right thing to do, but also because I believe that if we can get services and support right for this most vulnerable group of older adults, we’ll also transform it for the rest of the older population. The key principles of working with families and other carers, integrating our support across agencies and trying to enable as high a degree of independence as possible all apply to the wider population of older adults as well as to the cohort of patients diagnosed with dementia.
It is this approach that will see us succeed both in dealing with the numbers bulge and securing the far greater prize of providing coordinated person centred care and support for our older adult population. Then we’ll deserve the medal and have the moral victory!
Jeff Ace is Chief Executive Officer at NHS Dumfries and Galloway.

veryinteresting blog , explains the challenges we all have in the future
To deliver these key principles, improved information sharing, building and service redesign is essential, but patient centeredness (if thats a word) is a cultural transformation, changing our routine behaviours needs buy in and engagement from all levels of the organisation so I’m really pleased to read this blog
‘Care in the community’ has not worked well for our mental patients in the community with long waits for initial appointments and limited follow up appointments. I wonder why, if there is going to be an old age population explosion over the next 30 years, why we are building a hospital with even fewer beds when we currently have a bed shortage and are closing small hospitals and nursing homes are full? There is a shortage of carers in the community and they are struggling to cope to give 15 minutes of care 3 or 4 times a day. The concept may be one thing, but I fear the reality quite another.
I’d be interested in Mental Health colleagues’ reflections on the quality of their current service model as compared with the original configuration . With regards the new acute hospital, it will be 10 beds larger during the peak of our demographic ‘bulge’. The rumour that it’s smaller is persistent and persistently wrong!
Great blog Jeff and it clearly outlines the challenges ahead. Fantastic that you have completed the dementia champion training and are leading by example.I hope this encourages more people to follow suit.
Great blog Jeff, thank you. As one of the many ( you know who you are) who are perilously close to the bulge ( in more ways than one) this highlights important issues not only in relation to our professional lives as healthcare workers but as current and future recipients of health and social care. It Is essential that we get it right for our own sakes as well as the generations that follow.
Your reflections on dementia care are spot on. Your reflections on Welsh sporting successes are another matter all together of which I have no knowledge or authority on which to comment!
Linda, you make a good point that information on Welsh sporting success is very poorly communicated. We’re too modest for our own good.
It is a wonderful vision for the future but unfortunately all too late for us and my 88-year-old father for needs 24 hour care whcih we provide. On his last admission to hospital the nurse on the admissions unit was fantastic (not a dementia chmapion but someone who had studied in depth care of dementia patients) and worked long after her shift ended to record information such as how my father is sleepy in the morning, sometimes has swallowing difficulties, how his medication needs to be adminstered mixed in his food or in his drink, the help he needs to eat and that his replies to any question is not reliable because of the degree of his dementia. We said we would come in to feed him lunch and evening meals. Next day, he had been transferred to a ward, my husband arrived around noon to give my father his lunch and found him still asleep – no breakfast taken, no meds given. When he asked why they said it was because ‘he was sleeping’.
On previous admissions (and yes, he is becoming a frequent bed-user) we have begged staff to ensure he drinks enough – to no avail – battled to convince them he doesn’t like jelly. ‘Oh, but he said he did.’ No, you asked him if he wanted jelly and he either murmured yes or nodded his head – he does not have the ability to say he doesn’t like jelly. It takes a very long time for him to eat a meal so by the time he reaches his pudding the ice cream has melted into a puddle of gloop. I did mention that the community hospital has thermal pots which keep the ice cream frozen but was told there was no point in the staff requesting such a thing because of the cost.
Any medical intervention is rendered so less effective when the patient is not being kept well nourished and hydrated.
For families, every hospital admission of the person they care for becomes an exhausting battle.
Good blog Jeff, I’m looking forward to seeing the impact of your Dementia Champions training…I guess the challenge now is which of your colleagues does it next!