Dementia Awareness Week runs this year from 4 – 10 June. There are lots of events across the region supported by a wide range of individuals and organisations. This year, I’ll be promoting the use of a document called ‘This Is Me’ within acute hospitals and asking Dementia Champions and other colleagues across NHS Dumfries & Galloway settings to join in.
When someone with dementia comes into hospital, a care home or is receiving care at home, they and their family/friends may be asked if they have a ‘This is Me’ document.

What Is ‘This Is Me’?
‘This Is Me’ is intended for use by anybody with dementia, delirium or other communication impairment.
It aims to provide important personal information about the person from their perspective and those who know them best (family/caregiver) to help enhance the care and support given when the person is in an unfamiliar environment. It’s crucial that we understand the person as an individual and take their personal history into account, helping us to communicate and engage with the person, which in turn can help us to prevent/alleviate stress and distress.
What are the benefits of ‘This Is Me’?
For the person, their families/caregivers – if the person with dementia has memory and/or communication problems, then a ‘This Is Me’ guides and supports staff to provide care in a way that respects the person’s choices, preferences and routines. ‘This Is Me’ can be a great opportunity to ask and find out information, that as family members we may not know – provoking good memories and conversation. In addition, a ‘This Is Me’ or similar may reassure people with dementia and their caregivers that we see behind the dementia and respect that person.
For staff – for professionals, it can help us deliver person centred care, and importantly, reduce the times we ask for the same information – the detective work has already been done.

Where can ‘This Is Me’ be used?
‘This Is Me’ can be used anywhere, in hospital, care homes, in primary care, respite care and is offered during Post Diagnostic Support.
When should it be completed?
‘This is Me’ always offered during Post Diagnostic Support but can be completed at any time.
Are there issues around confidentiality/sharing this document?
The document is the property of the person and/or their main care giver – it is not a clinical document and does not belong to any professional or service, the person/care giver decides what information is included and shared.
Once completed, the document should be kept in a place that is easily accessible for those providing care, for example, at the bedside, in a care plan. The information can help staff understand the persons’ baseline abilities, lifestyle, routines, likes/dislikes and gives great opportunities for conversation and engaging with the person.
What happens to the form if/when the person is discharged or transferred?
As it belongs to the person, it should go with them on discharge/transfer, and it’s also useful to check with the person and /or their main carer that the information remains up to date and relevant.
Living Well with Dementia
It’s important to understand that many people are able to live well with dementia, leading active and fulfilling lives for years after they first experience difficulties and receive a diagnosis, but coming into hospital can be daunting for all of us, and for people with dementia , this can be a frightening experience.
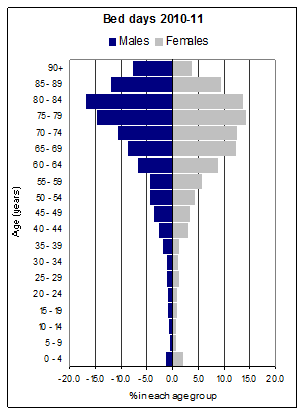
Whilst these days, a person with dementia may only be in hospital for a short time, how we communicate and support them will have an influence on the impact of the whole care experience and how quickly they can return home. We know that older people with dementia are more likely to be discharged to a care home than older people without dementia, have longer hospital stays and experience more falls and pressure ulcers.
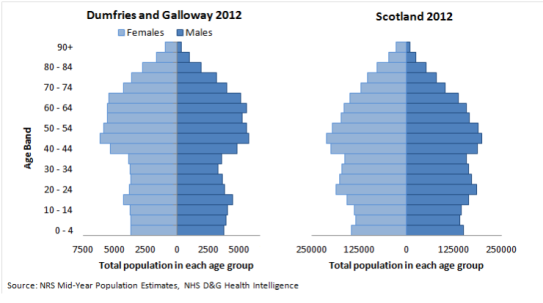
We know that in Scotland around 93,000 people are living with dementia and we think around 25% of all acute hospital beds are occupied by people with dementia (Alzheimer’s Research UK, 2018), yet mostly, people arrive into our services without a document such as This is Me even if they have one at home.
| “This is Me gives me golden information about an individual. The nuggets of information are priceless in helping to smooth the way to getting to know the person behind the dementia” | Gillian, Staff Nurse |
‘This Is Me’ is just one of a range of tools that can support centred care, Getting to Know Me, Life Story work and a wide range of personal profile tools are available, many online, helping professionals to see the person, not just the patient.

I ‘m keen to hear about your experience/s of using This Is Me in your workplace – please contact me or, if you would like more information about This is Me or would like a copy, please contact me at jgarton@nhs.net or 01387 246981.
Julie Garton, Alzheimer Scotland Dementia Nurse Consultant