NES AHP Career Fellowship Project by Karen Robertson, Occupational Therapist for Children and Young People
What does effective family-centred AHP neonatal and developmental follow up really look like? Part 2
Context
In Part 1 of this blog, I shared my perspective on the earlier stages of my NES AHP Career Fellowship experience. I discussed the opportunity and learning that has come from rich lived experience conversations with our local families who are accessing our AHP neonatal and developmental follow up service.
National guidelines informing neonatal and follow-up services advise around evaluating infants’ needs and promoting family-centeredness is a key recommendation (NICE 2017). Locally, our AHP neonatal and developmental follow up service is delivered by an existing pool of CYPF AHP’s and therefore capacity to do so remains limited, not ring-fenced and essentially fragile. Our AHP team wished to better understand what family-centeredness looks like within deliverable practice locally while recognising the constraints of our service. We wanted to explore the question;
“If we only have a limited time with this family and their baby, what will make the most positive impact for them now, and for the future?”
Policy informing healthcare in Scotland is underpinned by values such as partnership and integration and participation and engagement advocating continual improvement, creating the opportunity and environment to co-design services and honesty about priorities and constraints around what can be co-produced (Scottish Government 2016; 2022). This project has involved a response to families lived experience stories of participation to “further upskill AHPs and influence our future decisions about our ways of working and creating environments in which participation and participative relationships are possible.” (Scottish Government 2016)
Immersing in local lived experience
I recall feeling a sense of privilege to hold such rich information, as well as a responsibility to make sure it was handled with sensitivity, respect and managed in a way that would have the greatest impact for local families. Our next step was to make sure we could truly understand the wealth of information and what it could enable us to think about.
Key themes with underpinning sub-themes very quickly and consistently emerged from local lived experience stories which we immersed ourselves in as a team:
– Parenting on the Neonatal Unit
– Empowering families to access therapy support and the team around the family
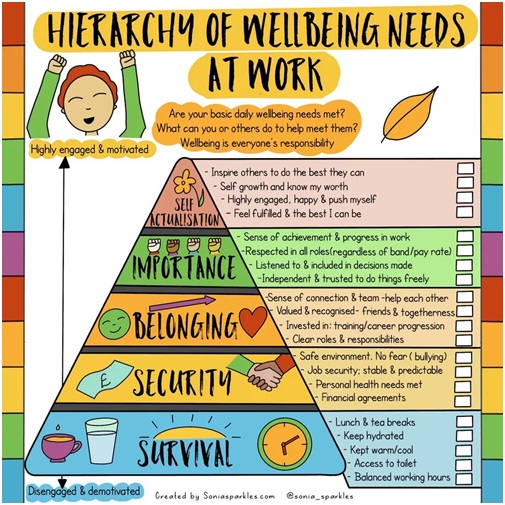
– Supporting parental wellbeing
– Communication and resources
– The focus of developmental follow-up appointments
– Empowering parents to advocate for their child beyond follow-up
Family-Centred & Family Integrated Care
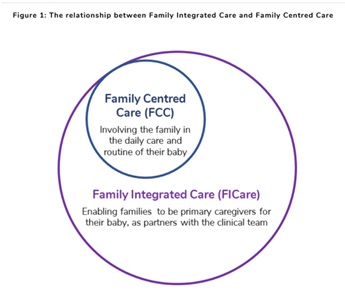
It was important to understand how local lived experience could be considered within wider frameworks informing on family-centred care. Within healthcare for the neonatal population, the British Association of Perinatal Medicine highlights the augmented nature of family-integrated care beside family-centred care. With the key being to not only ‘involve’ but to ‘enable families as partners in care’, as AHP’s our core skills within CYPF practice most certainly stood us in good stead for applying this framework to our neonatal and follow up practice.
(BAPM 2021)
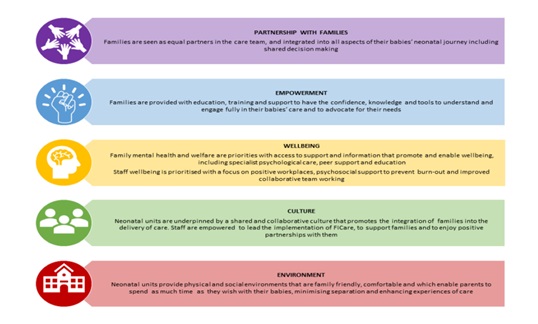
BAPM (2021) highlight 5 key principles of family-integrated care when working with this healthcare population within neonatal care.
Co-designing as a team
As an AHP team, we met to explore how we could realistically approach service improvement, within the scope of the project itself, our AHP roles and remit while holding on to the fact that our service is not ring-fenced and fragile. At this point, it felt enormous as all the data, with every parental quote felt important. This is when QI tools such as the high/low effort/impact scale became our friend to enable us to set realistic project goals. Another key asset was to consider what was within our circle of control and influence versus what would be reliant on wider complex systems.
Throughout December and January, we met as a team to collaboratively embed the local lived experience themes within each stage of our own AHP neonatal and developmental follow up care pathway.
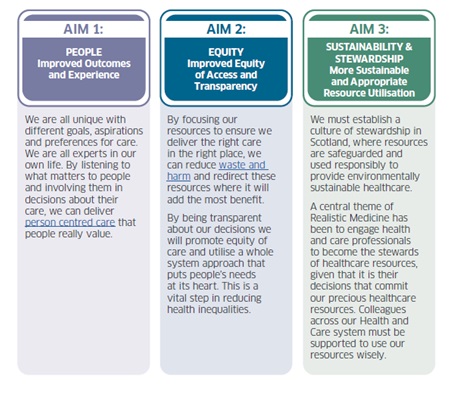
We aimed to approach our service redesign to….
- concentrate resource utilisation on where it is of most value and will have the most impact by responding to local lived experience
- reflect the underpinnings of AHP policy in Scotland & existing models of family-centred care for this healthcare population
- outline delivery of a realistic and sustainable local AHP service
Sense checking with families
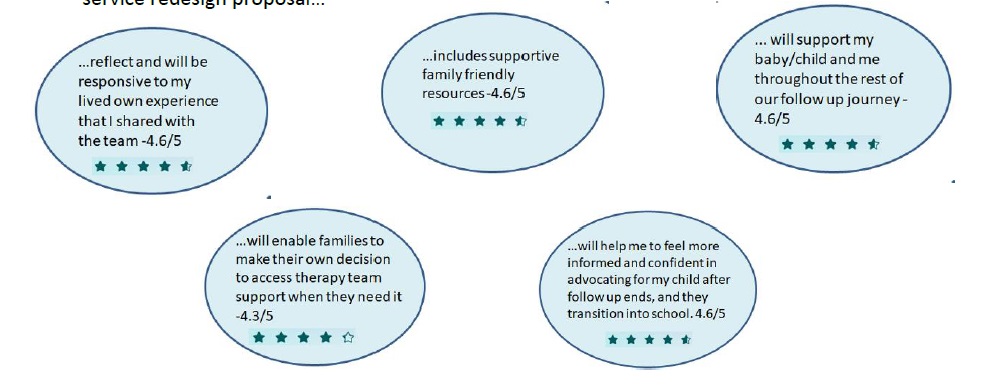
In February, we were delighted to host a ‘together session’ with participating families as an opportunity to share our thoughts so far on our service redesign based on their lived experience. This brought about a further opportunity to sense check with families that we were going in the right direction, and equally to prompt us to do so if we weren’t! Via a questionnaire following the event, 3 participating families shared with us that they think our service redesign proposal…
Key outcomes from the project
As an AHP team together with local families, we have been able to create
- an AHP service name, role and remit with an ability to be recognised for what we are and can do more of for local babies and families. We will be able to measure our impact and measure, manage and report on mitigation of risk with any incidence of unmet need.
- an AHP Neonatal Service Leaflet, outlining the roles and remit of the team, and to provide families with agency over when and how to seek support.
- A value based co-redesign proposal for an AHP Neonatal and Developmental Follow-Up Service based on lived experience of local families
- A journey map of resources for this population including available evidence based resources, and co-produced resources with visual supports across AHP team with family consultation.
If you would like to know more about this project, including the lived experience theme and sub themes, the co-redesign proposal our team are planning to implement and test and our long term vision, you can access a SWAY via this link: https://sway.cloud.microsoft/PoaVloHapya97zaH?ref=Link
So what’ next?
With supportive leadership across our AHP team leads and AHP management, we have permission to proceed with the next phase to test our service redesign proposal.
As well as being able to audit our requests for support quantitatively with this healthcare population, we have now embedded lived experience feedback opportunities for families into our core pathway to understand the impact.
Non ring-fenced AHP capacity means that service fragility is still a very real constraint facing CYPF AHP services. Our approach moving forward must be fluid, dynamic and responsive to needs of our local families balanced with wider CYPF service constraints.
In line with Ready to Act (Scottish Government 2016) in increasing appropriate access to interventions at universal and targeted levels of service as needed for improved well-being outcomes; we aim to explore how the journey map of resources can be made available for all neonatal families who are not receiving follow up.
Personal reflections – together truly is better!
As I approach the final weeks of the project phase, I am considering the impact that the experience has had on me. To mention my main learning outcomes would be a blog in itself, and so Ill skip to the headline; my most valuable (and unsurprising to me) learning outcome. This is that working together to co-redesign and co-produce really is better. When I review what we have achieved locally, I am full of pride to notice a part of each and every one of our local families and colleagues who participated and I thank each and every one of them. I would extend this understanding of co-redesign and therefore thanks to everyone locally and further afield who helped in any way to support his project. Service improvement relies on wider ingredients from supportive leaders to advising teams behind the scenes. Thank you!
If you would like to know more about the AHP Neonatal & Developmental Follow Up role, any aspect of our local practice for this health care population, or about this Career AHP Fellowship project, please get in touch.
Karen Robertson Karen.Robertson8@nhs.scot; @KarenOTRob
Blog part 1- AHPs across health and social care.
NICE 2017 – Overview | Developmental follow-up of children and young people born preterm | Guidance | NICE
Scottish Government 2016 – Ready to Act – A transformational plan for Children and young people, their parents, carers and families who require support from allied health professionals (AHPs)
Scottish Government 2022 – National Workforce Strategy for Health and Social Care in Scotland.