How many times have you heard a colleague or even you say “Thank goodness it’s Friday”?
Another busy week done and the weekend in sight. For the stroke and rehab patients on D7, we, as a therapy team, have tried to make a new meaning behind the phrase.
The National Clinical Guidelines for Stroke were updated this year (2023) and now state “People should receive at least 3 hours a day of therapy (therapist delivered) and should be supported to remain active for up to 6 hours a day”. This includes cardio-respiratory training once medically stable, for at least 30-40 minutes, 3-5 times a week for 10-20 weeks. Current research conducted by Chest Heart & Stroke Scotland (CHSS) has revealed a national crisis in rehabilitation, indicating that of the 1.1 million people in Scotland living with chest, heart, stroke and other long term conditions, less than half (45%) had accessed NHS rehabilitation services. CHSS is pushing the Scottish Government to improve services for people with long-term conditions and make sure they get the rehabilitation they are entitled to.
With this increased demand on acute AHP rehabilitation services within DGRI and only 8hours in a day, how do we as a team achieve this new guideline?
We as a therapy team put our heads together and this is where “Fun Friday” came into fruition.
Fun Friday is a small group session led by the OT’s, Physios and Rehab assistant practitioners and takes place on a Friday morning in D7’s therapy space. The session consists of a circuit style class which is created and individualised to maximise reaching the patient’s goals and aiding recovery. Person centred care is at the heart of the service. Patients who wish to take part in these sessions work on tasks that are important to them that include elements of both physiotherapy and occupational therapy.
The activities are varied depending on the patient’s ability and can range from seated activities to playing golf (in some sort of fashion). With limited resources at present we have had to be creative and experimental. The Therapists are challenged to be innovative and think up a whole host of activities to allow focus on the patient’s deficits e.g. sitting balance, standing balance, coordination, fine finger dexterity, weight transference, proprioception, cognition, problem solving, cardiovascular fitness, overall activity tolerance as well as to make it FUN.
We as AHP’s look forward to fun Friday but it is not solely for the patient’s and our enjoyment – There is an abundance of evidence out there to support group therapy.
In DGRI the wards are made up of single rooms, and although there are benefits to this, we have found that our patients can be at risk of social isolation and decreased motivation. A study conducted in 2017 “The effect of Group – Based Occupational Therapy on Performance and Satisfaction of Stroke Survivors” concluded that doing daily, craft, and mobility activities in the groups can affect the ‘performance’ and ‘satisfaction’ levels in stroke patients. Another article by Hillier, English et al (2017) stated by enabling individual’s to witness other stroke survivors rehab journey, in turn improved overall participation, motivation, level of activity and overall mobility outcomes and balance. According to research (Hartford, Lear and Nimmon, 2019), social support and social groups have a large role in the recovery process of patients who have had a stroke. Participant feedback from Hartford, Lear and Nimmon (2019), describe these groups as “nurturing” with a non-judgemental environment that allowed them to feel more confident and provided emotional support. Our patient feedback has reflected this, it has been inspiring to see these patients empower each other and become more confident.
Don’t just take our word for it, here is what the patients have to say…
We asked the patients attending weekly to complete a feedback form and here is a snippet of how they have found the class:
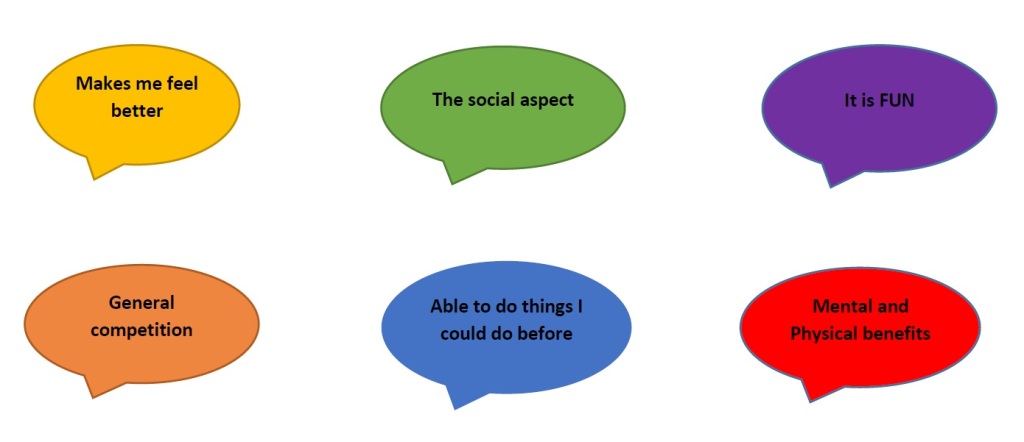
Overall, patients have fed-back that it has been good to practice and complete tasks that are relevant to their life and are practical.

As a small therapy team and a ward of 28 patients or even sometimes more due to bed pressures and double up rooms, we have had to work more efficiently and consider sustainability of the workforce to be able to meet the demands of the stroke and rehab guidelines and take the pressure off ourselves. Joint working is paramount in allowing timely but effective rehab which also reduces duplication of work.

Findings suggest recommendations for therapy frequency and intensity will remain unmet in many stroke units unless radical revision of therapist’s routine working practices are under taken. We may not be hitting the targets 100% but we as a therapy team are at least giving it our best go!
Written by Adele Parker (Specialist OT) and Isabella Bown (Specialist PT)
References:
Hartford, W., Lear, S. and Nimmon, L. (2019) ‘Stroke survivors’ experiences of team support along their recovery continuum’, BMC Health Services Research, 19(1). Available at: https://doi.org/10.1186/s12913-019-4533-z.
National Clinical Guideline for Stroke (2023) National Clinical Guideline for Stroke for the United Kingdom and Ireland, National Clinical Guideline for . Available at: https://www.strokeguideline.org/?_gl=1%2A1polfak%2A_up%2AMQ%2A_ga%2AMTg4NjE2MTY4My4xNjk4Njk1MTg5%2A_ga_EE3BZMVLRT%2AMTY5ODY5NTE4OC4xLjAuMTY5ODY5NTE4OC4wLjAuMA (Accessed: 28 October 2023)


