 This Beautiful young woman called ‘Holly Butcher’ posted her advice to the world 24 hours before she died of cancer.
This Beautiful young woman called ‘Holly Butcher’ posted her advice to the world 24 hours before she died of cancer.
This was her message for you…
“It’s a strange thing to realise and accept your mortality at 26 years young. It’s just one of those things you ignore. The days tick by and you just expect they will keep on coming; Until the unexpected happens. I always imagined myself growing old, wrinkled and grey- most likely caused by the beautiful family (lots of kiddies) I planned on building with the love of my life. I want that so bad it hurts.
That’s the thing about life; It is fragile, precious and unpredictable and each day is a gift, not a given right.
I’m 27 now. I don’t want to go. I love my life. I am happy.. I owe that to my loved ones. But the control is out of my hands.
I haven’t started this ‘note before I die’ so that death is feared – I like the fact that we are mostly ignorant to it’s inevitability.. Except when I want to talk about it and it is treated like a ‘taboo’ topic that will never happen to any of us.. That’s been a bit tough. I just want people to stop worrying so much about the small, meaningless stresses in life and try to remember that we all have the same fate after it all so do what you can to make your time feel worthy and great, minus the bullsh*t.
I have dropped lots of my thoughts below as I have had a lot of time to ponder life these last few months. Of course it’s the middle of the night when these random things pop in my head most!
1) Those times you are whinging about ridiculous things (something I have noticed so much these past few months), just think about someone who is really facing a problem. Be grateful for your minor issue and get over it. It’s okay to acknowledge that something is annoying but try not to carry on about it and negatively effect other people’s days.
2) Once you do that, get out there and take a freaking big breath of that fresh Aussie air deep in your lungs, look at how blue the sky is and how green the trees are; It is so beautiful. Think how lucky you are to be able to do just that – breathe.
3) You might have got caught in bad traffic today, or had a bad sleep because your beautiful babies kept you awake, or your hairdresser cut your hair too short. Your new fake nails might have got a chip, your boobs are too small, or you have cellulite on your arse and your belly is wobbling.
Let all that shit go.. I swear you will not be thinking of those things when it is your turn to go. It is all SO insignificant when you look at life as a whole. I’m watching my body waste away right before my eyes with nothing I can do about it and all I wish for now is that I could have just one more Birthday or Christmas with my family, or just one more day with my partner and dog. Just one more.
4) I hear people complaining about how terrible work is or about how hard it is to exercise – Be grateful you are physically able to. Work and exercise may seem like such trivial things … until your body doesn’t allow you to do either of them.
I tried to live a healthy life, in fact, that was probably my major passion. Appreciate your good health and functioning body- even if it isn’t your ideal size. Look after it and embrace how amazing it is. Move it and nourish it with fresh food. Don’t obsess over it.
5) Remember there are more aspects to good health than the physical body.. work just as hard on finding your mental, emotional and spiritual happiness too. That way you might realise just how insignificant and unimportant having this stupidly portrayed perfect social media body really is.. While on this topic, delete any account that pops up on your news feeds that gives you any sense of feeling shit about yourself. Friend or not.. Be ruthless for your own well-being.
6) Be grateful for each day you don’t have pain and even the days where you are unwell with man flu, a sore back or a sprained ankle, accept it is sh*t but be thankful it isn’t life threatening and will go away.
7) Whinge less, people! .. And help each other more.
😎 Give, give, give. It is true that you gain more happiness doing things for others than doing them for yourself. I wish I did this more. Since I have been sick, I have met the most incredibly giving and kind people and been the receiver of the most thoughtful and loving words and support from my family, friends and strangers; More than I could I ever give in return. I will never forget this and will be forever grateful to all of these people.
9) It is a weird thing having money to spend at the end.. when you’re dying. It’s not a time you go out and buy material things that you usually would, like a new dress. It makes you think how silly it is that we think it is worth spending so much money on new clothes and ‘things’ in our lives.
Buy your friend something kind instead of another dress, beauty product or jewellery for that next wedding. 1. No-one cares if you wear the same thing twice 2. It feels good. Take them out for a meal, or better yet, cook them a meal. Shout their coffee. Give/ buy them a plant, a massage or a candle and tell them you love them when you give it to them.
10) Value other people’s time. Don’t keep them waiting because you are sh*t at being on time. Get ready earlier if you are one of those people and appreciate that your friends want to share their time with you, not sit by themselves, waiting on a mate. You will gain respect too! Amen sister.
11) This year, our family agreed to do no presents and despite the tree looking rather sad and empty (I nearly cracked Christmas Eve!), it was so nice because people didn’t have the pressure of shopping and the effort went into writing a nice card for each other. Plus imagine my family trying to buy me a present knowing they would probably end up with it themselves.. strange! It might seem lame but those cards mean more to me than any impulse purchase could. Mind you, it was also easier to do in our house because we had no little kiddies there. Anyway, moral of the story- presents are not needed for a meaningful Christmas. Moving on.
12) Use your money on experiences.. Or at least don’t miss out on experiences because you spent all your money on material sh*t.
13) Put in the effort to do that day trip to the beach you keep putting off. Dip your feet in the water and dig your toes in the sand. Wet your face with salt water.
14) Get amongst nature.
15) Try just enjoying and being in moments rather than capturing them through the screen of your phone. Life isn’t meant to be lived through a screen nor is it about getting the perfect photo.. enjoy the bloody moment, people! Stop trying to capture it for everyone else.
Random rhetorical question. Are those several hours you spend doing your hair and make up each day or to go out for one night really worth it? I’ve never understood this about females
🤔.
16) Get up early sometimes and listen to the birds while you watch the beautiful colours the sun makes as it rises.
17) Listen to music.. really listen. Music is therapy. Old is best.
18) Cuddle your dog. Far out, I will miss that.
19) Talk to your friends. Put down your phone. Are they doing okay?
20) Travel if it’s your desire, don’t if it’s not.
21) Work to live, don’t live to work.
Seriously, do what makes your heart feel happy.
22) Eat the cake. Zero guilt.
23) Say no to things you really don’t want to do.
24) Don’t feel pressured to do what other people might think is a fulfilling life.. you might want a mediocre life and that is so okay.
25) Tell your loved ones you love them every time you get the chance and love them with everything you have.
26) Also, remember if something is making you miserable, you do have the power to change it – in work or love or whatever it may be. Have the guts to change. You don’t know how much time you’ve got on this earth so don’t waste it being miserable. I know that is said all the time but it couldn’t be more true.
Anyway, that’s just this one young gals life advice. Take it or leave it, I don’t mind!
Oh and one last thing, if you can, do a good deed for humanity (and myself) and start regularly donating blood. It will make you feel good with the added bonus of saving lives. I feel like it is something that is so overlooked considering every donation can save 3 lives! That is a massive impact each person can have and the process really is so simple.
Blood donation (more bags than I could keep up with counting) helped keep me alive for an extra year – a year I will be forever grateful that I got to spend it here on Earth with my family, friends and dog. A year I had some of the greatest times of my life.
..’Til we meet again.
Hol
Xoxo”


 This Beautiful young woman called ‘Holly Butcher’ posted her advice to the world 24 hours before she died of cancer.
This Beautiful young woman called ‘Holly Butcher’ posted her advice to the world 24 hours before she died of cancer. financial constraint. We started touring the region this week, meeting with teams to discuss these issues and ask them for their thoughts and ideas. It has been energising to hear from you all, there are lots of really good and simple ideas as to how we can change, but it is also apparent that there are many significant obstacles that it will take time to overcome.
financial constraint. We started touring the region this week, meeting with teams to discuss these issues and ask them for their thoughts and ideas. It has been energising to hear from you all, there are lots of really good and simple ideas as to how we can change, but it is also apparent that there are many significant obstacles that it will take time to overcome. Two words stick out to me, Innovation and Transformation. Both are necessary, both are hard, especially when we are busy, but both can be fun if we work together and support each other to deliver them. Done well they can make our lives less busy and our patients care safer and more person centred. But how can we achieve this? I know many people reading this will be thinking ‘Well, fill all our vacant posts and that will solve the problem’ and they may be right, but we know that is not easy and, whilst we cannot take our eye off the recruitment challenge, we need to do something else.
Two words stick out to me, Innovation and Transformation. Both are necessary, both are hard, especially when we are busy, but both can be fun if we work together and support each other to deliver them. Done well they can make our lives less busy and our patients care safer and more person centred. But how can we achieve this? I know many people reading this will be thinking ‘Well, fill all our vacant posts and that will solve the problem’ and they may be right, but we know that is not easy and, whilst we cannot take our eye off the recruitment challenge, we need to do something else. To create a compassionate culture, one in which we can thrive and transform our services, then we all need to demonstrate these simple behaviours. I urge you to ‘Hold the Mirror up’ to yourself and consider your behaviours not others. What can you do to improve your service, not what others can do to improve theirs.
To create a compassionate culture, one in which we can thrive and transform our services, then we all need to demonstrate these simple behaviours. I urge you to ‘Hold the Mirror up’ to yourself and consider your behaviours not others. What can you do to improve your service, not what others can do to improve theirs.



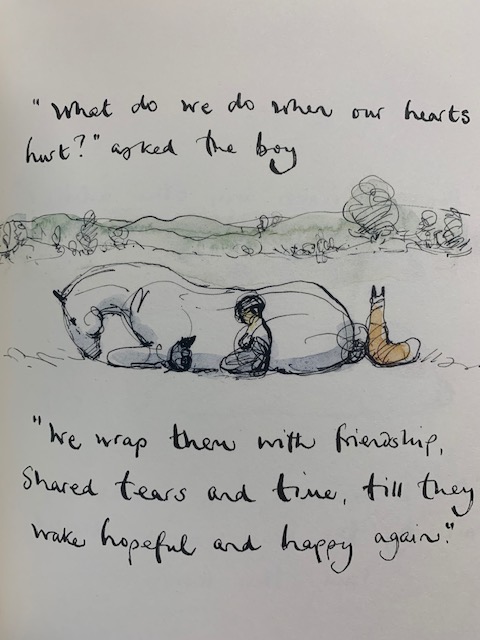
 When asked to submit something for the blog quite some time ago, the suggestion was that the subject be something that readers would find moving in some way. Recent press has been highlighting the degree of loneliness some are experiencing and how it can effect wellbeing physically, mentally and isn’t always visible to others.
When asked to submit something for the blog quite some time ago, the suggestion was that the subject be something that readers would find moving in some way. Recent press has been highlighting the degree of loneliness some are experiencing and how it can effect wellbeing physically, mentally and isn’t always visible to others.



















 Hello! My name is Alison! I work as a Clinical Psychologist in the Clinical Health Psychology Service; the final member of the team to blog this month as part of our service promotion! Part of my role within this job is to help individuals and their families manage psychological distress caused by or maintained by physical health problems. Of course as a psychologist I do this at a professional level, but do we always need to be a psychologist to provide psychological care to those who need it?
Hello! My name is Alison! I work as a Clinical Psychologist in the Clinical Health Psychology Service; the final member of the team to blog this month as part of our service promotion! Part of my role within this job is to help individuals and their families manage psychological distress caused by or maintained by physical health problems. Of course as a psychologist I do this at a professional level, but do we always need to be a psychologist to provide psychological care to those who need it? went off to a football match that afternoon as planned. Twelve hours later after a trip to A&E (“just to be on the safe side”) our worst fears were confirmed. I’m happy to say that after a successful angioplasty he made a great recovery, but at the time we both pretty devastated. I was beside myself with worry. My stomach churned and my thoughts raced out of control “Was he going to die?”, “Would he have another?”
went off to a football match that afternoon as planned. Twelve hours later after a trip to A&E (“just to be on the safe side”) our worst fears were confirmed. I’m happy to say that after a successful angioplasty he made a great recovery, but at the time we both pretty devastated. I was beside myself with worry. My stomach churned and my thoughts raced out of control “Was he going to die?”, “Would he have another?” I felt overwhelmed. How would I help my husband to cope if I was struggling myself? I had no one to talk to and could not voice my fears to my husband who needed me to be strong. As a Clinical Psychologist with many years experience working with people who have experienced distressing life events, I knew that my thoughts and feelings were normal but I was at a loss as to how to help myself.
I felt overwhelmed. How would I help my husband to cope if I was struggling myself? I had no one to talk to and could not voice my fears to my husband who needed me to be strong. As a Clinical Psychologist with many years experience working with people who have experienced distressing life events, I knew that my thoughts and feelings were normal but I was at a loss as to how to help myself. He simply smiled, gave me a cup of tea and said, “It’s hard isn’t it? How are you doing?”
He simply smiled, gave me a cup of tea and said, “It’s hard isn’t it? How are you doing?” Dr Alison Wren is a Clinical Psychologist for the Clinical Health Psychology Team at NHS Dumfries and Galloway
Dr Alison Wren is a Clinical Psychologist for the Clinical Health Psychology Team at NHS Dumfries and Galloway